Categorized under "My Photo Journal"
Tuesday, October 1, 2013
Sunday, September 8, 2013
5th Term School of Medicine Information and Advice. Saint George's University. Grenada, West Indies. + BSCE 2, OSCE, and NBME Information.
Congratulations,
you have made it through term 4~! You now have 18 weeks left before
completing your basic sciences and progressing onto clinical
training. The hard part is over (at least while you are on the
island for basic sciences) and you now have a little more breathing
room as compared to the previous term. The workload is much more
manageable and you can fill up your free time doing what you please.
I personally chose to focus 30% of my time for studying SGU courses
and 70% preparing for the boards. I treated the entire 5th
term as a preparation for the step 1 and filled up whatever free time
I had to studying for it. I will write about my entire board
preparation and USMLE experience in a later post.
Unlike the previous term advices, where I wrote immediately after finals, I completed term 5 around 3 to 4 months ago. I have forgotten many of the little nuances but will do my best to paint a good picture this term.
Intro
to Clinical Medicine – 3 units
You can expect lectures to be of the same caliber as that of CPD, being that both courses are coordinated by the same department. I believe only 4 lecture were required in order to comply with SGU’s rules. However, you do have to attend almost all the small group sessions and hospital visits, and you can only miss 2 if you want to receive 5% credit for professionalism. In regards to the exams, I do not believe it reflected the contents of lectures but rather on small group discussions. Our midterm and final was weighted 15% and 25%, respectively. OSCE was weighted 40% of our grade.
There
is small group session that meets once a week for 90 minutes. Your
group members will be pretty much consistent throughout all the
courses in term 5 (by last name in alphabetical order). During these
sessions, you will review over a case and discuss what questions you
should ask, physical exams to perform, what labs and special tests to
order, and the differential / final diagnosis. This is followed by
two quick multiple choice questions that aren’t directly related to
the case. You will receive an electronic copy of the case with
detailed explanation of the answers each week. Topics cover
cardiology, endocrinology, psychiatry, respiratory, rheumatology,
etc. I studied mainly from these electronic notes and just flipped
through last terms CPD notes. I believe the latter was unnecessary
and was not the most efficient use of my time.
On a side note, you have short (less than 2 hours) small group sessions three times a week in 5th term (ICM, BSFCR, and either Pharmacology or Pathophysiology).
My favorite portion of this course involved the one-time a week visits (Monday – Thursday) to the hospital. You meet up with your group at 8am in front of Charter Hall (near the bus stop). Your group will take the newer air conditioned SGU buses to the main hospital, psychiatry unit, or private physician’s office. You will spend each of the 9 weeks rotating through various specialties within medicine (internal medicine, emergency medicine, pediatrics, female medicine, male medicine, anesthesiology, surgery, psychiatry). Your group may not have the opportunity to experience all the specialties since you will spend 4 rotations in internal medicine. There was also one SIM lab where we engaged in various activities with the human dummies.
Your group of 6 students will be divided into two groups during most of the rotations. You will take turns interviewing patients, maybe doing physical exams, and then presenting the case to the doctor. I personally felt that the majority of the physicians were very passionate and eager to teach.
We
had 2 case write-ups (worth 5% each) which consisted of documenting a
complete history, physical examination, differential diagnosis,
assessment, and problems list. Below is a sample of my case write-up
which received a 98%.
Name: Brian Fung
Student ID Number: A00------
Date of Patient Visit: ------ --, 2013
Patient Address: -------------, Grenada
Location of Patient: True Blue General Hospital – Surgery Ward
Name of Clinical Preceptor: Dr. ---------- ------------
History
History Of Present Illness
D.A.,
is a married obese 44 year-old Afro-Caribbean female cooking
assistant, that presents to the general hospital surgical ward with a
three week history of constant painless hematuria. D.A. stated that
she had constant “Coca-Cola colored” urine for the previous two
weeks before seeing blood. The patient stated the hematuria occurred
suddenly without any precipitating factors. There was no change in
her usual activities or diet which brought about the hematuria. This
is the first time the patient has seen blood in her urine. D.A.
states that there is no pain or any other symptoms associated with
the hematuria. D.A. does not report feeling any nausea, weakness,
dizziness, or general malaise. D.A. does not appear to be in acute
distress or have any signs of a fever or infection. She states that
the blood looks like “washing fish” initially and “turns
brighter red” towards the end of urination. D.A. reports that
nothing she does alleviates or aggravates the hematuria. The
frequency of her urination did not change from its usual three to
four times a day.
Past
Medical History
D.A.
repots no previous surgeries, trauma, illness, and is up to date on
her immunization. D.A. reports not having any major childhood
illnesses. D.A. has been to the hospital each time giving vaginal
births to her eight children without any complications. She states
she had one planned abortion ten years ago because she did not want
more children at that time. D.A. reports being allergic to dust and
flour since it causes her face to become “puffy” especially
around the eyes after handling flour or cleaning the house. She
reports that the “allergic” reactions have never been serious
enough to warrant a visit to the doctor or hospital. She reports no
airway constriction or dysphagia associated with her allergic
reaction. She does not take any medications for her “allergies”
which occurs about two times every week for as long as she can
remember. D.A. is currently taking migraine medication prescribed by
her doctor six years ago as needed. She does not know the name of
the drug and does not currently have the prescription bottle with
her. She reports having migraines after giving birth to her last
child six year ago. D.A. mentions being on a course of antibiotics
four months ago and that the infection has since resolved without any
sequelae. D.A. is currently taking multi-vitamins for her hair since
she believes they may be getting less shiny and brittle. D.A. had a
PAP smear performed a year ago with inconclusive results due to her
“cleaning down there” too thoroughly. She was asked to go back
again but did not follow through with the practitioners’
recommendation. D.A. has never been tested for STD or breast cancer.
D.A. was thirteen years old when she had her first menstruation.
She states that her cycles are normal and that bleeding last for five
days with the first two being the heaviest. She reports feeling some
abdominal cramps while she is menstruating but not enough to warrant
a visit to the doctor or medications. She has no history of diabetes
or hypertension. D.A. reports having blood work done a year ago with
the results stating that she had high cholesterol. She is not
currently taking medications for her high cholesterol.
Family
History
D.A.
70 year old mother is alive with no chronic illnesses. Her 80 year
old father was diagnosed with prostate cancer a few years ago. She
has four sisters with no history of chronic illnesses. She has eight
children all of whom have no history of chronic illnesses. D.A.
mentions that her husband is well with no history of chronic
illnesses. D.A. reports that no one in her family has ever
experienced hematuria.
Social
and Personal History
D.A.
is a cooking assistant. She reports not ever drinking water because
it tastes bland and that she only drinks coffee or coke. She
normally eats rice, chicken, stew, and fruits. D.A. informs us that
she does not eat pork because she does not like the flavor of the
meat. D.A. mentions that her co-workers complain she puts too much
salt in her cooking. D.A. says she did not ever exercise. D.A.
reports no history of smoking, drinking, or recreational drug use.
She is currently sexually active with her husband and does not use
any form of contraception. D.A. claims not having any other sexual
partners other than her husband.
Review
of Systems
D.A.
reports feeling sharp stabbing and throbbing headaches once a week
ever since giving birth to her last child six years ago. She is
currently taking migraines headaches as needed. D.A. began wearing
glasses a year ago because she was unable to read after dark and that
things started becoming blurry. She does not report and changes in
her smell or taste. D.A. does not report any history of tinnitus.
D.A. reports difficulty swallowing because she feels pain in the
epigastric region. She mentions that she can’t eat after 7pm
because of the associated burning sensation when lying down. She
also reports that the burning sensation radiates to her back. D.A.
reports that the epigastric pain can be elicited with superficial and
deep pressure to the sternum as well. She reports feeling the
similar pain in the epigastric region when she lifts heavy objects.
D.A. reports the pain sometimes restricts deep breathing. She
mentions “frothy” vomit occurs if she eats too late at night
before going to bed. D.A. does not report any history of angina or
shortness of breath with activity. She does not have any history of
bowel movement issues and reports going regularly once a day. The
color of her stool is brown with a firm consistency. She has no
history of hematemesis, hiatal hernia, retching or use of NSAIDs.
She mentions occasional diarrhea that usually subsides in a few days.
D.A. reports feeling bloating pain around the umbilical region in
the past but has since resolved with no complications. D.A. reports
having episodes of anxiety that began seven months ago that prevents
her from sleeping. She reports feeling hot and sweaty, with muscle
aches all over her body, along with dizzy spells and feeling terrible
as symptoms associated with these attacks. D.A. does not report
experiencing general weakness or ataxia other than during the
attacks. These symptoms warranted a visit to her doctor who
informed her that she may be experiencing menopause. D.A. does not
report any joint pains. She does not report any changes in her skin.
D.A. does not bruise easily or have any history of skin ulcers.
D.A. does not report any numbness or lower extremity swelling. D.A.
does not report any recent changes in her appetite, weight, or energy
level.
Physical Examination
D.A. heart rate was 90 beats per minute, symmetrical with amplitude of +2. The character of her pulse as determined on her brachial artery was a rapid upstroke with a rounded summit followed by a slower downstroke. Her respiration rate was 22 breaths per minute. The rise of her chest was symmetrical in size and shape. There were no signs of respiratory distress, no use of accessory muscles, and no apparent intercostal retractions. Her systolic blood pressure as determined by auscultation in the supine position was 110 mmHg. D.A.’s blood pressure as measured in the supine position was 138/90 mmHg. Osler’s sign was negative. D.A. did not have a fever. D.A. did not report having any pains.
Initial
Observations
D.A. is a middle-aged Afro-Caribbean female. She is oriented in person, place, and time. She is aware and responsive to the environment. D.A. is obese weighing roughly 200 to 250 pounds at a height of approximately five feet four inches. D.A. does not appear to be in acute distress. She does not appear to be lethargic or have any signs of fatigue. D.A. has a urinary catheter in place with the urinary bag filling with bright red urine. D.A. has a 0.9% glucose saline IV drip. D.A. has no obvious sign of cyanosis or jaundice. D.A. has no signs of cachexia. She does not appear to be in respiratory distress. There is no fluid discharge from her nares, ears, and eyes. D.A. has no apparent signs of edema. She is propped up on a pillow for comfort to speak to our group. D.A. does appear to have engorged veins in her neck and no apparent deviation of her trachea from midline. Her hands and feet do not appear to be trembling.
D.A. is a middle-aged Afro-Caribbean female. She is oriented in person, place, and time. She is aware and responsive to the environment. D.A. is obese weighing roughly 200 to 250 pounds at a height of approximately five feet four inches. D.A. does not appear to be in acute distress. She does not appear to be lethargic or have any signs of fatigue. D.A. has a urinary catheter in place with the urinary bag filling with bright red urine. D.A. has a 0.9% glucose saline IV drip. D.A. has no obvious sign of cyanosis or jaundice. D.A. has no signs of cachexia. She does not appear to be in respiratory distress. There is no fluid discharge from her nares, ears, and eyes. D.A. has no apparent signs of edema. She is propped up on a pillow for comfort to speak to our group. D.A. does appear to have engorged veins in her neck and no apparent deviation of her trachea from midline. Her hands and feet do not appear to be trembling.
Examination
of Relevant System
D.A.
finger nails were negative for Shamroth’s sign. There were no
changes in the consistency of her nails. There were no signs of
pallor, palmar erythema, or Dupuytren’s contracture. Asterixis was
not elicited on physical examination. The arms had no sign of muscle
wasting, bruising, or scratch marks. Her palpebral conjunctiva was
normal pink in color. Her sclera had no yellowish discoloration.
D.A.’s eyes did not appear sunken. Parotids were not enlarged.
There were no signs of xanthelasma around the eyes. Fetur hepaticus
was negative. Her tongue did not appear enlarged and the surface of
her tongue was of normal texture. No signs of cyanosis were noted.
There was no discharge, signs of dehydration, ulcerations,
pigmentations, or white lesions noted in her oral cavity. Hair
pattern was consistent with D.A.’s age and gender. No apparent
signs of weight loss or gain. D.A. had stretch marks around the
lateral and anterior aspects of her abdomen. No spider naevi or
scars were noted on her abdomen. D.A. did not have any signs of
peripheral edema.
D.A.
was attached to a urinary catheter. Upon inspection of her abdomen,
it was noted that she had symmetry in both size and shape. There
were no apparent lesions, masses, or swellings. Her umbilicus was
not protruding. The color of D.A.’s skin was consistent with her
ethnicity. No signs of hernias were noted. No signs of distended
veins or arterial pulsations were noted. The movement of her abdomen
was normal during respirations.
Auscultations
for bowel sounds were normal. No high pitched or sounds were
detected. No signs of bruits, friction rub, and venous hum were
noted upon auscultation. Superficial palpation did not elicit any
tenderness, guarding, rigidity, or superficial masses. No enlarged
masses were detected during deep palpation of the abdomen. The aorta
was slightly left to middle and was approximately 3 cm wide. Liver
and spleen were not enlarged upon palpation. Both right and left
kidneys were difficult to assess due to the patients adipose tissue.
Bladder was not assessed because the group did not want to disrupt
the urinary catheter. Costovetebral tenderness was negative
indicating no pyelonephritis.
Percussion
of D.A.’s abdomen yielded tympanic sounds. The liver border was of
normal size during percussion. Sound did not change while percussing
the spleen to assess for organ enlargement. Fluid wave sign was
negative indicating that D.A. did not have ascites. Murphy’s sign
was also negative indicating no acute appendicitis. Boa’s sign was
negative indicating no acute cholecystitis.
Differential Diagnosis
Bladder neoplasia
Acute nephritic syndrome
Systemic
lupus erythematosus
Assessment
D.A., is an obese 44 year-old Afro-Caribbean female cooking assistant, that presents to the general hospital surgical ward with a two week history of “Coca-Cola” colored urine followed by a three week history of constant painless hematuria. She reports that her urine becomes redder towards the end of urination. D.A. has no other symptoms associated with her hematuria. D.A. did not have any change in her diet or activities of daily living prior to the onset of hematuria. She reports that nothing makes the hematuria better or worse. D.A. reports that no one in her family has a history of hematuria. She mentions that her 80 years old father was diagnosed with prostate cancer a few years ago. She has no history of sexually transmitted infections. D.A. has eight children delivered through natural birth. D.A. has been having moderate to severe intermittent migraines for the past six years since giving birth to her last child. Her migraines are being managed by medications prescribed by her primary care physician. D.A. reports having “allergies” to dust and flour due to face swelling especially her eyes swelling upon contact. The allergies have not been severe enough to warrant a visit to the doctor or hospital. D.A. reports feeling attacks of anxiety, heat, sweating, general agitation, and an inability to sleep during these episodes that began seven months ago. She reports that her primary care physician believes it is symptoms related to menopause.
D.A.
had no abnormal peripheral signs of abdominal diseases upon physical
examination. Examination of the abdomen yielded no positives for
pathological diseases. It was noted that D.A. had stretch marks
around the lateral and anterior aspect of her abdomen due to adipose
tissue. D.A. has a urinary catheter in place with the urinary bag
filling with bright red urine. D.A. has a 0.9% glucose saline IV
drip. Due to the above asymptomatic clinical presentation and
negative physical exam findings, it was determined that D.A. most
likely had bladder neoplasia. D.A. also was negative for pain and
pyelonephritis and with no fever. The diagnosis was further enforced
by the color and increase in blood toward the end of urination
indicating hematuria of bladder origin.
Problem list
Bladder neoplasia
Gold
standard for diagnosis is cystoscopy. Urine cytology can also be
obtained. Staging and grading of the cancer following detection of
neoplastic cells is the next appropriate step. Treatment includes
transurethral resection and can be followed up with immunotherapy,
radiation, and/or chemotherapy for invasive disease.
Acute
nephritic syndrome
Diagnosis
would include detection of auto-antibodies such as antineutrophilic
cytoplasmic antibodies, anti-GBM, or anti-streptolysin O titre.
Levels of protein in the urine along with signs of renal
insufficiency can also be assessed. Management and treatment would
include plasmapheresis, steroids, and immunoglobulins.
Systemic lupus erythematosusDiagnosis would include CBC, serum creatinine, and urinalysis with microscopy. Other lab test include ESR results, complement levels, liver function test, and autoantibody tests. Management and treatment include either biological or non-biological DMARDs, NSAIDs, and corticosteroids.
Pharmacology
– 6 units
I would say that pharmacology was the only class I really studied this term. With that being said, this class was fairly easy in terms of its content. The only difficult aspect had to do with the sheer volume of its material. I guess that can be said of most medical school courses, but this one especially rung true.
Your grade is determined from three midterms and attendance points taken during each small group session. The attendance points will be added as bonus points to the numerator of your midterm scores.
I personally found the small group facilitators in pharmacology to be high quality and felt the sessions were especially educational / informative. You do have to prepare beforehand and you can’t use your notes during the small group sessions. With that being said, I do strongly feel that you get out what you put in. The clinical tutors will go around the group asking questions from the assignment you were supposed to do prior to each session. There is no need to worry if you don’t know the answer to something…someone in your group will chime in and help…and if no one knows the answer, the clinical tutor will give you the answers. There was a short written quiz at the end of every session which was not graded.
Like I said earlier, this was really the only class I studied for during 5th term. The first midterm had about half the drugs tested (you start with learning concepts) as compared to the second and third exams (list and list of drugs). I personally felt the anti-microbial section was most demanding in terms of pure memorization. One saving grace was that exams were not cumulative and many drugs were repeated again in subsequent tests but for a different medical purpose. You must focus on learning the mechanism of action, pharmacokinetics (CYP450, CYP2A1 inducers and inhibitors), clinical use, when drug is indicated for use (elderly, renal dysfunction), BIG contraindications (child, pregnancy, alcohol, renal failure, liver dysfunction) and BIG side effects (torsades de pointes, hypokalemia, tendon rupture, teratogenic effects, etc.)…basically everything that was presented in the PowerPoint lectures.
You will be given a note packet with details of all the drugs covered during class. I made the mistake of reading the note packets…looking back I would highly suggest only using that as reference if you truly do not understand something. If I were to do it over again, I would focus ONLY on the lecture handouts (PowerPoint slides) and take note on what was emphasized during lectures. I purchased Katzung & Trevor’s Pharmacology Examination & Board Review book, but did not end up using it for this course. Students who have used this book have told me the questions were good but more challenging than our course demanded. Some students also used the Lippincott’s Pharmacology textbook (one of the many books I did not ever use as part of our welcoming book package in term 1) which explained pharmacology and the mechanisms of action in much greater depth.
Speaking of lectures, most students in my class went in the beginning of the term but found that their time would be better spent watching the lectures at their own leisure (I watched at 2X the speed). We were encouraged to go to lecture but mandatory attendance was not required for our class. The in-class quizzes (We were not required to attend lecture during these clicker sessions; videos would still be recorded and the answers posted online later that day) emphasized what the instructors want you to know from the lectures. If you are unsure of how your studying is coming along, I would suggest doing the quizzes to see where you stand. The exam questions were all FIRST ORDERED and the in-class quizzes reflected the level of difficulty. One aspect of this department I was particularly appreciative of was that after midterms, they would send a message out with questions the majority of the class got wrong and explain the concepts behind the questions and answers.
Pathophysiology
– 12 units
Lectures in pathophysiology were structured much in the same way as pathology. You had visiting professors come and give lectures on topics they had clinical experience in. The topics covered were exactly the same as in pathology except with a dash of physiology (you can get that just from the course title). The quality of lecturers was similar to the ones in pathology. I must say that a couple of professors, especially the course director, did an AMAZING job in explaining the higher yield topics such as cardiology and endocrinology. We had to learn a bunch of facts in pathology but were never given the reason why. In pathophysiology, for the most part, we learn the how. I believe this is very important because it allows one to reason out certain things rather than just memorizing a bunch of random information. With that being said, I personally felt that only a few topics covered in pathophysiology accomplished that.
Your grade in this course is based off three midterms, NBME score (12% of grade), and professionalism points (based off attendance in small group). I feel that in term 5, the school really wants you to pass and leave the island, whereas in 4th term, I got a sense that they gave it their last hurrah to decel students. The reason I am saying this is because of the ridiculous bonus points we received in our 5th term courses. This is especially true for pathophysiology where we received an additional 8, 9, and 5 percent increase in our grades for exams 1, 2, and 3, respectively.
Small group sessions were rotated between pharmacology’s small groups (met once a week). You will get very comfortable with seeing the same faces every single day, being that most students will have the same group in every lab. You will receive around 4 to 5 cases each week and will have to answer them to prepare for these sessions. I felt the cases did not benefit me but rather took time away from my studies.
In terms of how I prepared for this course…I must say that I didn’t really study from the lecture notes / handouts (except the topics covered by the course director and a couple other high quality professors). I focused the majority of my time studying from First Aid, BRS Physiology, Pathoma, and doing USMLE World questions. I did however tailor my studies according to the topics covered in the course. For instance, if the topic covered this week was neurology, I would crack open said books and study the topic at hand. I found that doing USMLE World questions benefited me the most for the pathophysiology examinations and the USMLE Step 1 exam. I will go into more details on my USMLE Step 1 experience in a later post.
Basic
Science Foundation and Clinical Reasoning – 2 units
BSFCR was just an extension of the pathophysiology course. We met once a week on Fridays for small group and went over cases that were posted on Sakai. I strongly felt that this course was a waste of time…I learn better when I can sit down and digest the material by myself rather than having someone say it aloud. A lot of students in my term read their answers directly from the computer and then mentally checked out the rest of the time. Here is how we divided the cases each week in our group.
Your
grade is based off of 3 exams (20 questions in each exam taken
immediately before the pathophysiology exams), 8 quizzes,
professionalism points (attendance for small group), and NBME (6.25%
of your grade). You take an in-class written 10 question quiz (not
multiple choice, you must have correct spelling and no abbreviations)
each week on Friday at 1pm. After you finish, you sit around until
your lab session starts which will be either at 2pm or 3pm (lab times
switch between groups halfway into the semester).
BSCE
Two
Like the BSCE one, the questions on this exam encompasses all the material you have covered thus far. This time however, the exams last the entire day from 9 to 5 with a lunch break in between. There are a total of 400 questions divided into two blocks of 200 questions. I treated this exam as a training session for my endurance…nothing more. The exam was not difficult and I believe almost every single student passed (Cutoff for pass / fail was class mean minus ½ a standard deviation).
OSCE
Taking a history and doing physical examinations shouldn’t be as foreign to you now. I practiced for two days with 3 other students and felt that was more than adequate. Make sure you get your timing down for the history taking (8 minutes). The second OSCE was similar to the first except this time around you have 3 histories and 4 physical exam stations which consisted of 2 majors and 4 minors (2 minors per station). The main difference this time around, was that instead of telling you to do certain physical exams, you were given a short vignette. For example, a major station would have a case about a patient with Grave’s disease. You would be expected to do a complete thyroid examination. Another example would be a patient with ALS where you would be expected to test the upper and lower motor neuron system (in this case, they will tell you to omit certain things in the vignette). Minors would be like a patient with low back and leg pain. You will be provided physical examination materials when you enter the room, and in this case a paper clip, vibration fork, and cotton ball. Hint: Look at all the instruments they have provided for you in the examination room. You will be required to use all of them.
Other examples:
Majors
Inspect, auscultate, percuss, and special tests of abdomen
Inspect, palpate, and percuss posterior chest
Percuss and auscultate the heart and special test
Knee exam and special test
Venous insufficiency examination and special tests
Percuss and auscultate posterior chest for respiratory system with special test for diaphragm paralysis
Ear with special tests
Neurological examination of lower limb – 1 leg numb, 1 leg weak
Inspect and palpate pericardium
Abdomen with appendicitis
Cranial nerve examination for nerves exiting the pons and medulla
Examine axial skeleton – patient had been in car accident
Oral cavity
Minors
Tests for meningitis
Peripheral respiratory signs
Lower limb arterial system with special tests
Lower limb venous system with special tests for DVT
Extra ocular eye musclesMini mental examination
Examine the sinuses
Evaluate for tunnel vision
Lumbar spine with sciatica
Nose examination due to foreign body
Taking patients vital
Pyelonephritis
Hip pain with special tests
Lymph nodes
Cerebellum examination
Carpal tunnel syndrome with special tests
JVP
Peripheral abdomen
Examine for signs of right heart failure with hepatojugular reflex
Eye fundoscopic exam
Ear examine and special hearing tests
Parietal cortex examination
Peripheral signs of thyroid disease
Palpate axillary and epitrochlear lymph nodes
Shoulder muscle examination
Examine and palpate parotid gland and its ducts
Visual acuity and visual field examination
Examine lumbar spine including special tests
Anterior eye chamber
Tests for hepatosplenomegaly by palpation and percussion
Patient history
Gout
Infertility with vaginal discharge
Patient with headache and family history of hypertension
Man with STI
Perimenopausal female
Progressive dysphagia to solids with weight loss
Woman with arthritis
Woman with nausea and breast pain
Man who failed while in toilet with blood in stools
Diabetes with history of sexual dysfunction
Diarrhea
Chest pain
Tuberculosis
Pregnant patient
RLQ pain, spotting, nausea, with last menstrual period 2 months ago
Patient with HIV and severe diarrhea
Menopause
Cough with phlegm, cold, fever, chills, and sharp flank pain
Older male patient with penile discharge
Older female with heartburn
Burning on urination
Tired, fatigued, and shortness of breath
Patient with unable to have children presents with yellow vaginal discharge and history of abortion 10 years ago
NBME
– CBSE Comprehensive Basic Science Examination
Let me start off by saying that I strongly believe in taking full advantage of this experience. The NBME-CBSE examination was taken near the end of the semester. It was 4 blocks, with 46 questions per section. Our class was divided into 5 groups and sat for this exam throughout a period of one weekend. A representative from NBME came to administer the 4-hour exam. You should receive your scores in about 1 week (MyCourses My Sites NBME Gradebook2) and your score breakdown in about 1 month (via SGU e-mail).
I believe this was an invaluable experience that one should take seriously. I used this test as a baseline for the USMLE Step 1. The score I received allowed me gauge my current level of preparation and to also set a realistic goal for myself. According to the NBME-CBSE score interpretation guide, two times out of three, a student’s true proficiency on the Subject Examination will be +/- 3 points from the actual level of proficiency.
I will use own marks as an example. I received a score of 81, which was equivalent to 227.5 or 94th percentile ranking. My level of proficiency at that time predicted that my USMLE Step 1 results should fall in-between 84 to 78, which equates to 235 to 220, respectively. In my case, the USMLE Step 1 score I received was 243, a little over 6 points greater than my NBME-CBSE results or 98th percentile ranking. I will write about my USMLE Step 1 experience in a later post.
Wednesday, July 17, 2013
Grand Anse Beach, The Complete Package. Grenada, West Indies.
From what I've collected, Grand Anse Beach is most favored and best all around with tourist, students, and locals alike. Lined with resorts, water sports businesses, restaurants, and most importantly, beauty, Grand Anse Beach is truly your one stop center for everything there is to enjoy in life. With it's convenient location next to the main road, you can get to and fro from place to place with ease. Also, the main grocery and hardware store of the island, IGA Super Value and Creative Do it Your Best, is within walking distance for all your needs.
Note: Grand Anse beach, compared to all other Grenada Beaches will most of the time be the busiest beach around. It's pretty quiet during off peak times away from holidays and weeks that cruise ships are in town.
Location
From cruise landing, make your way to main bus terminal in town. Take the #1 bus (2.50EC/3EC Holidays) and stop next to vendors (right next to roundabout and Gitten's Pharmacy, ~5-10min). Walk toward lifeguard tower. There are many access points to beach. You can pretty much walk through any of the resorts to get through to the beach.
From SGU, take Grand Anse bus to last stop (pavilion right next to beach).
What to Do on Grand Anse Beach
-relax on rental chairs placed on beach front by resorts for a little fee
-scuba dive with aquanauts (they offer snorkelling/water boat rentals and PADI internationally recognized certification courses)
-snorkel
-sleep
-all resorts welcome people to come in and purchase cocktails (no need to be an actual guest)
-eat at their beach front restaurants (Umbrellas is the main spot to go offering burgers, fries, nachos, smoothies, fish, sandwiches, hot dogs, beef ribs, desserts, and alcoholic beverages). Other restaurants include Ali Babas, and IGA Grocery food court options.
-purchase souvenirs from spice/craft market (information, adjacent to beach) or resort shops
-resort dining open to outside, call for reservations
-get a massage
-jog or early walk along shoreline (beach is 2 1/2 miles long)
-sunbathe
-hang out under shaded trees
-get married
-photography
-hire a boat guy to take you to some great snorkelling sites
-SGU Significant Others almost always hold their midterm social here
Tips
-don't forget to bring lots of sunscreen
-always stay hydrated
-depending on day, beach vendors may be active... if not interested in what they're selling, a simple "no thank you," will often do the trick
-don't forget to bring your camera or waterproof camera
Grand Anse Beach Resort Information
(For reviews on all resorts listed down below, visit TripAdvisor. Most resorts also have their own website. Google them for more information).
Hotel Resorts Located on Grand Anse Beach
Coyaba
Allamanda
Spice Island
Siesta Hotel
Blue Horizons Garden
Grenada Grand
The Flamboyant
Grand Anse Beach Palace
A Little Ways from Grand Anse
Mt. Cinnamon
Kalinago
La Luna
Located at the Beginning of Lance Aux Epines
Calabash
Next to Saint George's University
True Blue Bay
Next to Maurice Bishop International Airport
Grenadian by Rex Resorts
 |
| Ghost Rock Discovered by my Friend, Angela. |
Categorized under "Things to do, Sights to See"
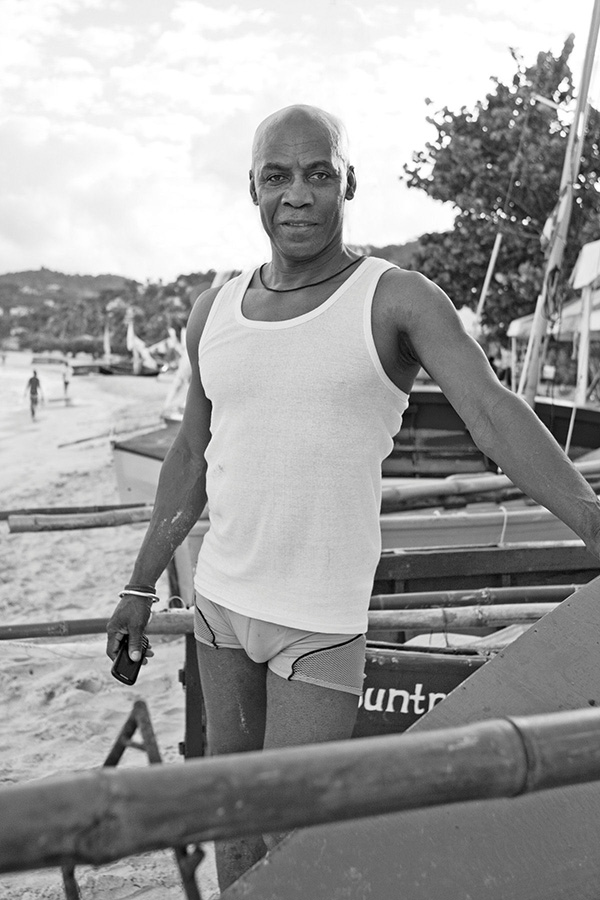
Yearly Event- Grenada Sailing Festival Workboat Regatta
Event Held: Late February-Beginning March
Information (sailing week 2014)
-two day event
-races within own classes: Gouyave Sloop, Gouyave Canoe, Sauteurs, Woburm, Petit Martinique, Carriacou
-big community celebration with performances, food, and lots of beer/fresh cut coconuts
-Location: Grand Anse Beach next to lifeguard tower. From SGU, take the Grand Anse bus to last stop (pavilion at beach).
-20th anniversary held in 2013
This event is one of my favorite annual events in Grenada because it, in my eyes, represents everything Grenada is: proud, hardworking, community/family oriented, a country that knows how to work the kitchen (men, women, and children alike), and beautiful.
Categorized under "Things to do, Sights to See"
He has straws if you ask for one and if you would like to taste the jelly inside, try finishing up your juice there so he can cut it open for you. Unless you have a machete at home, these guys are so tough to open up. Even throwing them off the second floor of your apartment building just won't do.
Subscribe to:
Posts (Atom)
39th Anniversary of Grenada's Independence
2.7.13 St. George's Downtown and National Stadium Grenada, West Indies. © Katherine Fung, All rights reserved. Grenada, The ...

-
Veggie Sprout Burger- A Vegetarian Treat
-
If there's one thing I love about Grenada... (ok, maybe three things), It has to be its' people, beauty, and produce. Local...


























.jpg)

.jpg)












.jpg)














